Introduction
Plantar fasciitis is a common and often painful condition that affects the plantar fascia, a thick band of tissue that connects the heel bone to the toes. Millions of people all around the world experience it, making it one of the most common reasons of heel pain. Plantar fasciitis can have a substantial negative impact on a person’s everyday activities and quality of life if it is not treated.
Repetitive tension and severe pressure on the plantar fascia are the usual causes of plantar fasciitis. This can happen for a number of reasons, such as excessive walking or jogging, wearing unsuitable footwear, having high arches or flat feet, being obese, or partaking in activities that subject the feet to repetitive stress. Runners in particular are more prone to getting this ailment than other athletes.
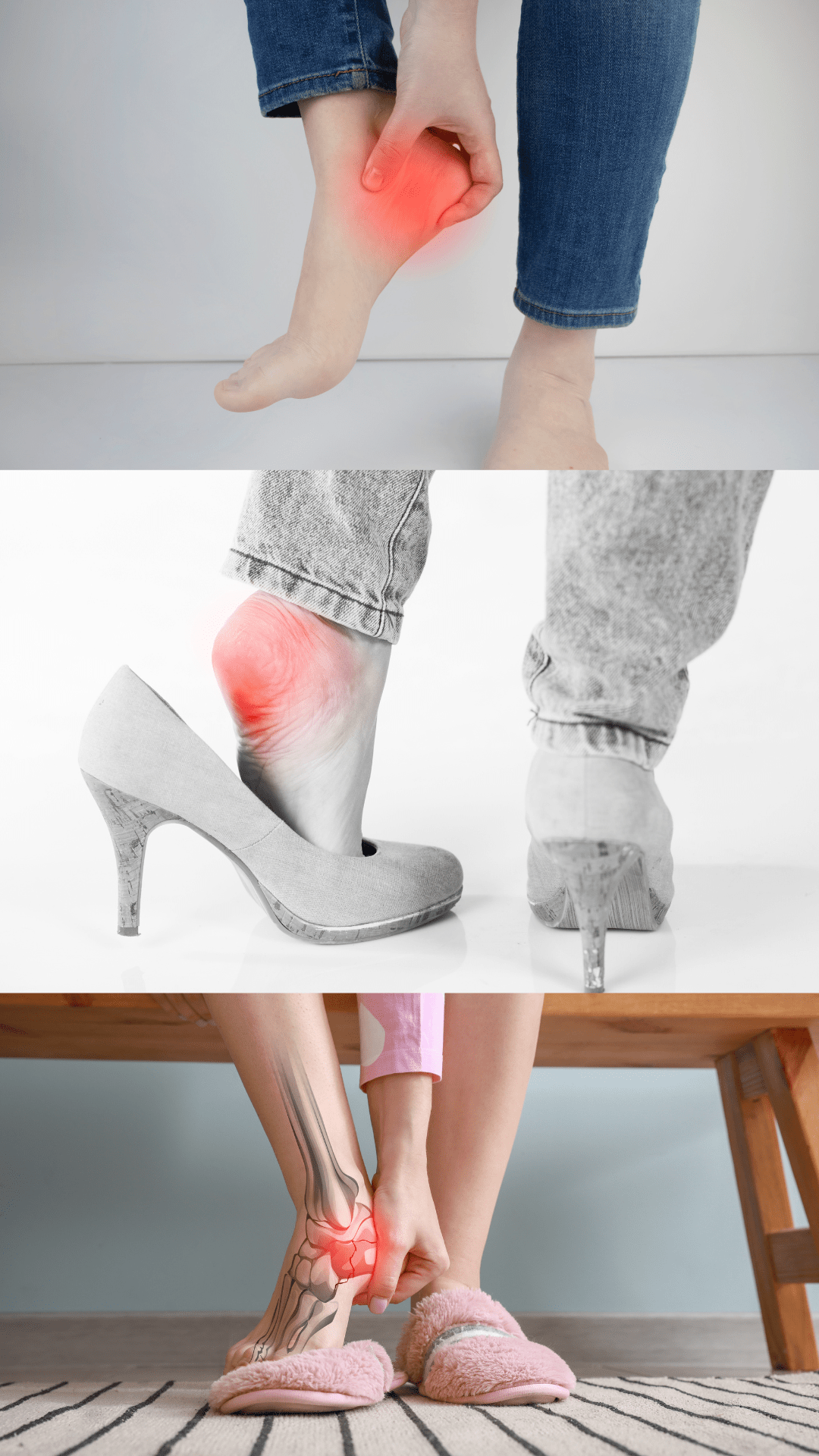
The defining sign of plantar fasciitis is a stabbing, severe pain in the heel, which is frequently at its worst when taking the first steps in the morning or following extended periods of inactivity. As the foot warms up, the discomfort might go away; but, after prolonged standing or strenuous activity, it might come back.
To effectively manage plantar fasciitis, early intervention and appropriate care are essential. Despite the fact that there are many different forms of treatment, physiotherapy is increasingly recognised as a powerful strategy for reducing pain, encouraging healing, and avoiding recurrence.
You can take proactive measures to manage the problem successfully and regain your mobility and foot health by comprehending the causes of plantar fasciitis and how physiotherapy is used to cure it. Let’s explore plantar fasciitis in more detail and see how PT can significantly impact your road to recovery.
What is Plantar Fasciitis & What are the Symptoms?
The plantar fascia is a broad band of connective tissue that runs along the sole of the foot, supporting the arch and absorbing shock when walking or running. Plantar fasciitis is characterised by inflammation and irritation of the plantar fascia.
When the plantar fascia experiences prolonged, excessive stress or tension, plantar fasciitis results. There are a number of causes for this, including:
- Excessive or repetitive activity: Prolonged standing, jogging, or leaping can put tension on the plantar fascia and cause irritation.
- Foot mechanics: High arches, flat feet, or other aberrant foot mechanics can change how forces are distributed in the foot, which in turn puts more strain on the plantar fascia.
- Inappropriate footwear: Plantar fasciitis can develop as a result of wearing shoes without adequate arch support or cushioning.
- Age and weight: Middle-aged people and those who are overweight or obese are more likely to develop plantar fasciitis because the added weight puts additional strain on the feet.
The most typical sign of plantar fasciitis is severe heel discomfort, especially when getting out of bed or after rest periods. After prolonged standing or physical exercise, the pain could also get worse. Additional signs can include:
- Stiffness and limited mobility in the foot
- Pain that improves with activity but returns later
- Tenderness or inflammation in the heel or arch area
To diagnose plantar fasciitis, a healthcare professional, such as a physiotherapist, should perform a thorough examination.
The Role of Physiotherapy in Treating Plantar Fasciitis
Physiotherapy is a key component of effective care and rehabilitation when it comes to managing and treating plantar fasciitis. At Achieve Health, we use a variety of methods and interventions that are tailored to each person’s particular requirements in order to treat both the condition’s symptoms and its root causes.
1. Initial Assessment and Diagnosis
A thorough assessment and diagnosis serve as the foundation for all subsequent treatment steps. The mechanics of the patient’s feet and lower limbs, as well as their range of motion, strength, and general movement patterns, will be thoroughly assessed.
2. Individual treatment plan
There is no one-size-fits-all method of treating plantar fasciitis with physiotherapy. An individualised treatment approach is necessary for the best results because every patient’s situation is unique and their causes are unique to each individual’s anatomy – so Dr Google isn’t your friend!
3. Treatment
Plantar fasciitis can be efficiently managed using a variety of treatments and interventions offered by Achieve Health. In the course of treatment, the following methods may be used:
- Strengthening exercises
- Mobility and stretching exercises
- Myofascial release
- Deep soft tissue massage and frictioning
- Shockwave
- Joint Manipulation and Mobilisation
- Biomechanical Assessment leading to possible Orthotic device prescription
- Gait analysis and Correction.
Physiotherapy seeks to promote healing, enhance foot mechanics, and avoid recurrence while reducing discomfort, inflammation, and tension in the plantar fascia. We will go through the advantages of physiotherapy for plantar fasciitis in greater detail in the following part, emphasising the beneficial effects people can anticipate from using this strategy.

Benefits of Physiotherapy for Plantar Fasciitis
- Pain relief and Healing
Pain relief and healing from plantar fasciitis is one of the main objectives of physiotherapy. Physiotherapists can aid in reducing inflammation, releasing muscular tension, and relieving pressure on the plantar fascia by combining targeted exercises, manual treatment, and other procedures as touched on above.
- Increased Flexibility in the Foot and Ankle
The plantar fascia, calf muscles, and other foot and ankle tissues are all targets of particular stretching and mobilising exercises used in physiotherapy. The plantar fascia is less stressed as a result of these stretches, which also enhance range of motion and general foot mechanics. Enhanced flexibility can also help reduce the likelihood of further injuries by improving walking patterns and shock absorption.
3. Enhanced Stability and Strength
The foot and lower leg muscles can be strengthened as part of physiotherapy programmes for plantar fasciitis. These exercises increase total foot stability and give the plantar fascia better support by focusing on the intrinsic foot muscles, calf muscles, and other supporting tissues. Enhancing the function of the foot by strengthening weak muscles can assist transfer forces more uniformly across the foot, easing pressure on the plantar fascia.
4. Recurrent Injury Prevention
In addition to treating the current case of plantar fasciitis, physiotherapy aims to stop flare-ups in the future. Physiotherapists give patients the tools they need to take charge of their own treatment and avoid the recurrence of plantar fasciitis by addressing biomechanical problems, addressing incorrect gait patterns, correcting them, and educating patients on the best footwear and training methods. This long-term strategy guarantees long-lasting pain relief and enhanced foot health.
Beyond only pain alleviation, the advantages of physiotherapy for plantar fasciitis include holistic care that tackles the underlying reasons, fosters healing, and gives patients the tools they need to take an active role in their recovery. Patients can experience better foot function, more mobility, and an overall higher quality of life thanks to individualised treatment strategies.
Tips for Self-Management and Prevention
We at Achieve, love to educate. We can give advice and tips so individuals can actively participate in their recovery and reduce the likelihood of future episodes. Below are some of the areas we can advise on;
- Proper Footwear Selection and Support
- Orthotics
- Stretching and Strengthening Exercises for Plantar Fasciitis
- Lifestyle Modifications to Reduce Strain on the Foot
- Regular Follow-ups with a Physiotherapist for Maintenance and Prevention
Conclusion
Heel pain and suffering are brought on by plantar fasciitis, a common and frequently crippling ailment that affects the plantar fascia. However, people can effectively manage and treat plantar fasciitis with the use of physiotherapy, finding comfort, improving foot function, and avoiding recurrences in the future.
For those with plantar fasciitis, physiotherapy has a number of advantages, such as pain relief, better foot mechanics, protection against recurrence injuries, and long-term management plans for the condition. People can actively participate in self-management strategies, take preventive measures, and support their own healing and foot health.
For a precise diagnosis and a personalised treatment plan, it is essential to seek professional assistance from a physiotherapist. Physiotherapists are qualified and knowledgeable to evaluate foot mechanics, provide individualised treatment plans, and offer advice for long-term maintenance.
Always remember that the key to treating plantar fasciitis is early intervention. Getting physiotherapy treatment as soon as possible will help with pain management, stop the problem from getting worse, and hasten the healing process.
Consult a physiotherapist if you have foot discomfort or plantar fasciitis symptoms in order to get a proper diagnosis, effective treatment, and advice on self-management strategies. You may overcome plantar fasciitis and regain your mobility and foot health with the proper strategy and preventative care!
